Paul Manley Back Pain and RSI Clinic
Paul Manley, M.A.O.(Manip), Registered OsteomyologistFor muscle and joint problems

RSM (Royal Society of Medicine)
Specialist in the treatment of Musculo-skeletal problems
Location: 8-10 Boston Place, Marylebone, London NW1 6QH
Next to Marylebone Station, Main line trains and Bakerloo line
19/01/2026
Glossary of back pain terminology.
Below is an illustrated glossary of commonly used back pain, spinal and pain terminology which has been compiled by me from the phrases and wording commonly used by patients to describe their symptoms and disease names.
Many of the terms used are non-medical or pseudo-medical. Many of the terms used are inter-changeable with others. It is the purpose of this glossary to inform those in need of help how to understand some of the terminology in common use. My definitions and explanations are drawn from the experience of addressing issues and confusion over pain terminology for many years.
1. Global descriptors
Inflammation
- Inflammation
is the response by the body to damage. It is
the beginning phase of the repair mechanisms.
It feels hot to the touch, sometimes there
is some swelling around the area of repair
due to the build of repair fliuds and damage
collecting white blood cells, platelts
and other cellular substances. Sometimes
and are of swelling will become so taut
that it pressurises the perimeter of the
swollen area and blocks the passage of
repair fluids away from the area of repair.
In this indurated state the repair will
slow down and will be more likely to form
scar tissue in the long-term. thus, we
will tend to rub the area better. If it
is too delicate we tend to cool the area
with cold applications. Some of us take
anti-inflammatory drugs to varying degrees
of good to 'no-help at all' types of responses.
Aspirin is very effective as an anti-inflammatory
but much under-rated due to the over promotion
of other less efficacious remedies, most
notably paracetamol. Some of the supposed
pain killers available without prescription
are too dangerous to be let loose on the
public. The common perception of the dangers
of over the counter drugs is that because
they are available without prescription
they must be safe.
- Inflammation
of the joints,
muscles and tendons are more possible when the body is 'building up' to an infection. During the first few days of an infection, most commonly, flu and colds, the body switches on its inflammatory response system. During this period any area of the body which is on the verge of inflammation will respond by getting more inflammed. The whole body is in repair mode and anything which needs it gets repaired. The trouble is that it often gets 'out of hand' whilst the metabolism switches into a 'collapse, rest and repair' mode such additional pain and discomfort is most unwelcome. The patient will often present as an acute pain in the spine and then 3 days later they have come down with an infection of some sort. The additional effect of the swelling of the bone marrow in order to produce more white and red blood cells, stretches the membranes covering the bones, producing that awful acheing across the whole body, nerves are more sensitive, pain more acute, we crave peace and rest. Any loud noise or excessive commotion can profoundly disturb the ill person, so we quite naturally tiptoe around them. This has the added dimension of allowing them to feel your caring and your love and respect. We are complex beasts y'know. Often the feelings of the carers can become inflammed at these times. Stress, frustration and fear all take their toll on both the patient and carer.
Aching
- Muscles
ache for various reasons
- Tiredness
Muscles are fuelled just like any engine, and just like any fuel, it can run out. The muscle needs rest whilst the body restores its fuel supply to the muscle. During this state the lactic acid and other metabolites which accumulate as the 'spent fuel' will easily induce a cramp, spasm or acheing in the muscle. The lacitic acid is drained away by the circulation of blood back to the heart and lungs which occurs in all tissues. If the area concerned is already tight and thererby, constricted in its blood supply, the the crampy state will persist for longer. At times this can be a continuous state where we 'must be careful not to strain a certain parts of our structure'. We are usually aware of these areas which need some protection, but not always. Areas of tension will build up come what may. Such muscle adaptations to functional requirements is what makes us such rapid learners of new mental skills as well as of manual skills. Thereby being a blessing in disguise, an instrument for change.
- Tension
Muscles can be in a continual state of activity, even when supposedly 'at rest'. The resting tone of any muscle of the skeleton will change according to its typology i.e. phasic or postural but, primarily according to the amount of regular work we ask the muscle to do. If the type of work is of a static or stabilising, supportive role, then the muscle resting tone will increase and the fibo-elastic make-up of the muscle will adapt to become thickened and shorter. In this state they will be much more prone to acheing, muscle pulls, tears, strains and inflammations due to the poor blood supply to the now dried up, leathery tissue which used to be a part of fully functioning muscle. I say 'part of' because it is more usual that the deep fibres of the muscle will undergo this type of change most readily. The more superficial fibres become redundant in the functioning of the muscle, and will shrink to add mechanical advantage to the deeper fibres. - Over
exertion
a short term repair response to the stretching of the membrane surrounding the muscles ( sarcomyalgia ). This results in the acheing experienced following unusually strenuous or new exercises. The pain is a direct result of the rapid expansion and ulitimate growth of the muscles which produced the exercise. - Changes
in brain stem respiration control
can lead to inappropriate breathing patterns which will make our body either too acidic or too alkaline. In either extreme, the body becomes more prone to muscle acheing. It is wise to be aware of the balance of our own pH. The most common state, by far, is one of acidity. Use water to alkalise if dehydrated, Andrews liver salts or a very alkaline spring water, are ideal buffers for your blood. A buffer will absorb the acid in your blood and digestive tract. Panic attacks whilst in pain can only serve to make the situation worse.
- Tiredness
Lethargy
- The feeling
of tiredness, overwhelming lack of motivational
ability, depression and an uncaring attitude
to the neccessities of life. Can be due to
geberal metablolic mal function or the need
to recharge our batteries. Adrenalin exhaustion
is a common cause amongst workaholics and
worry-aholics. Convalesence is often the
answer. A period of two to three months of
careful attention to rest and sleep as well
as establishing a more regular daily schedule
will often be sufficient to rejuvenate us.
Anemia, low blood sugar, shock and long term
emotional trauma can lead to lethargy.
Stress
- We are
often told that our pains are due to stress.
Whilst this label is often used as an excuse
for poor physical diagnosis, there is interplay
between the state of the nervous system and
pain perception. When adrenaline is high
due to stress, any pain will be amplified.
The fact is that in the brain stem there is a nerve centre which governs our perception of pain. Theoretically, if this centre were set to maximum we would be in agony all over our body, if switched off, we would be numb. Morphine can achieve this latter effect.
The nervous system and its' pain perception settings fluctuate according to various factors. We all have areas of repair or ache which will remain subliminal ( below the level of conscious perception ) until other factors raise the overall activity in the nervous system. An example of this is when, for instance, you have sprained your ankle and have just achieved a comfortable position of rest for the ankle. Someone then comes into your vicinity who is screaming and shouting about something concerning them. The immediate result is that your ankle suddenly becomes intensely painful and you must beg them to be quiet. The sound input and angst behind their indelicate assault on your senses raises the overall excitation of your nervous system and you are instantly in agony. Hence when people are in pain, they need peace and quiet in order to recover. Thus the appearance of a person in pain can be one of attention seeking and manipulation of those around us. However, the term is immensely overused due to the total inability of some doctors to diagnose sources of physical pain.
Then you have the added complication of inadequate treatment for the common causes of pain. When a course of treatment fails to bring relief the patient then questions the diagnosis, treatment and their own mental state. I have found that all too often the source of pain is obvious and its' treatment simple to provide. However there are many people who end up labeled as neurotic, due simply to the ineptitude of the professionals involved in their case. This adds to their stress, amplifies their fears and multiplies the uncertainty about a successful cure being possible.
Sleep
- Sleep
is more than rest. It actively repairs our
body, restores the nervous system to a quieter
state. It enables our conscious-unconcious
state to stand back and observe our stresses
and lives.
It is normally considered that sleep prepares us for our awake life and is often relegated to being an unwelcome interference with that precious awake life. I could posit the opposite: that we wake in order to sleep. During sleep, our dreams are often more vivid and intense than most daily events. We can die in our sleep from nightmares, we can make love to the girl of our dreams, we can sun ourselves on Bondai beach or be chased by demons. If the whole purpose of our existence is to experience life, then surely sleep provides an adequate alternative to the humdrum of our daytime lives.
Have you ever asked yourself a question as you are passing into sleep. I usually ask myself a question about solutions for practical, technical problems which have been bothering me for lack of a solution. Usually a computer or clinic related matter. Almost without fail I will come up with the correct answer or at least another angle on the puzzle on waking.
This view of sleep upgrades the value of sleep not only as reparative on the physical and emotional levels but also a valued state, to be cherished as equally as being 'awake'.
If sleep is denied, the whole body becomes more painful due to the effect on the brain stem. How many times have we been in pain all day, aching and tired, we have a ten minute 'catnap' and most of our pain disappears? When the sleep cycles i.e. circadian rhythms, are out of cycle due to jet lag or late nights it affects all of our metabolic cycles negatively. The Pineal gland governs the overall timing of these intricately interdependent metabolic cycles. Each organ repairs itself in its' own time slot. The liver and kidneys repair late at night whilst we sleep. If we deny our organs this repair time or disrupt their repair sequences we may be putting out the garbage in empty sacks whilst the garbage builds up in our kitchen. Sleep is the best thing that we can do for ourselves on all levels of our existence. Perhaps the waking life simply fuels us with food, experiences and the money to buy a roof over our head and a bed beneath our bones.
2. Typology
These descriptions of the three main body types are readily observable in real life and are therefore a useful reference system. We are all manufactured in accordance with these descriptors. We all have a different combinations of these factors.
- Fibrous
- The muscles are thick and heavy, skin taut, tend to be stocky, joints tight and have less range of motion
- Watery
- The muscles lack tone, skin spongy, tend to be round in shape, joints very flexible with extreme range of movement.
- Elastic
- The muscles are high tone and compact, skin smooth and elastic, tend to be slim and graceful, joints flexible with good range of movement
3. Reflex resting tone
- The excitability of the nervous system varies from person to person. You can be high, medium or low in terminology of reflex response. This is best evaluated by using a reflex hammer, testing the femoral, ankle, triceps, biceps and brachioradialis jerk responses. Thus the typologies mentioned above can exist along with such reflex settings as their long term state. The higher the reflex tone the easier it is for a person to put on muscle. A high reflex tone also means that a small pain can become huge, spreading along the nerves and exciting any older, subliminally irritated or repairing injury, long forgotten. By the same means the high tone person generally repairs more quickly. The reflex setting of the individual if too low can delay repair and pain dulling responses. The low tone muscles adapt less rapidly. There are dramatically different response times for musculo-skeletal repair in the two extremes.
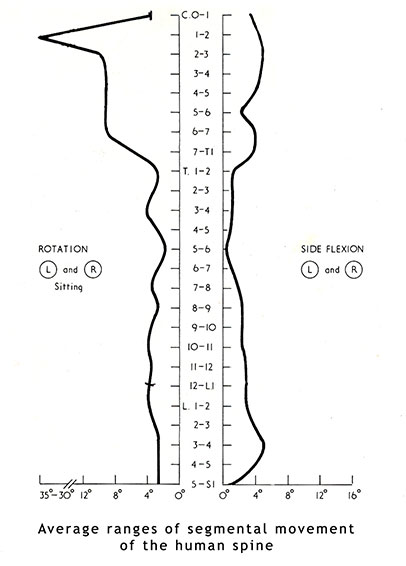
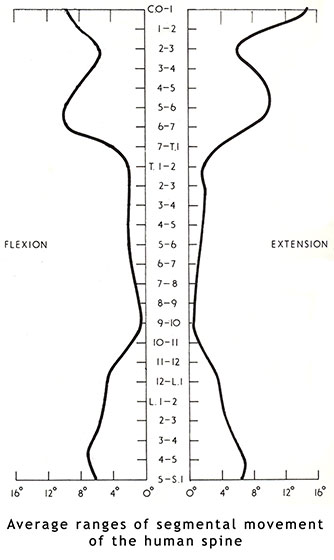
4. Disc related terminology
Some of the terminology commonly used to describe the condition include herniated disc, prolapsed disc, ruptured disc, and the misleading expression "slipped disc." Other terminology that are closely related include disc protrusion, bulging disc, pinched nerve, sciatica, disc disease, disc degeneration, degenerative disc disease, and black disc.
- The popular term "slipped disc" is quite misleading. An intervertebral disc, being tightly sandwiched between two vertebrae, cannot actually "slip," "slide," or even get "out of place." The disc grows together with the adjacent vertebrae. A disc can be squeezed, stretched, and twisted, all in small degrees. It can also be torn, ripped, herniated, and degenerated, but it cannot "slip."
- Most disc herniations occur when a person is in their thirties or forties when the nucleus pulposus is still a gelatin-like substance. With age the nucleus pulposus changes ("dries out") and the risk of herniation is greatly reduced. At the same time osteoarthritic degeneration, especially in the facet joints, makes its inroads.
- Cervical disc herniations occur in the neck, most often between the sixth and seventh cervical vertebral bodies. Symptoms can affect the back of the skull, the neck, shoulder girdle, and shoulder blade. But are most likely to cause severe pain in the shoulder, arm and hand.
- Lumbar disc herniations ( lower back ), occur most often between the fourth and fifth lumbar vertebral bodies or between the fifth and the sacrum. Symptoms can affect the lower back, buttock, back thigh, and may radiate into the lower calf and foot. Usually pins and needles on the outside of the foot accompanied by aching in the low back and buttock is a good indicator of some degree of disc compression.
- Great care must be taken to assess the role of secondary spasm. The muscle reactions to a non-disc related primary irritant and their resultant spasm in the buttock can put direct pressure on the sciatic nerve. Even a small amount of pressure in this area will mimic a disc protrusion. In such cases it is best to calm the secondary ares and then to decompress the disc area. The reflex hammer will reveal much about the source of irritation to the sciatic nerve. The femoral nerve which runs down the front thigh is more usually affected by deep muscle tension over L1 - L3.
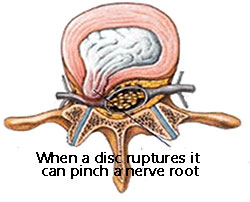 Inflammation
following a local microtear of
muscle or ligament will commonly cause irritation to the
nerve root.
Inflammation
following a local microtear of
muscle or ligament will commonly cause irritation to the
nerve root.
I find that most pains which have been diagnosed as disc herniations respond very well to my techniques. Normally I see the patient within a few days of the pain having occurred and calm the whole thing down. I then proceed over a few sessions to lengthen the compressed areas of the spine specifically over the area involved and generally along the whole spine and legs, front and back. This usually does the trick within a couple of weeks. On the other hand, I have seen many who have been suffering for many months and who have had all sorts of help, drugs, exercises, manipulation, physio with little or no response. It is wonderful to be able to help these cases so dramatically. Conventional medical diagnostics has not and should not attempt to place inadequate labels onto conditions which can consist of multiples of variables, as complex and individual as your face.

MRI of spine:
This degree of disc bulging of L4 and L5 (rare) will definitely cause symptoms but often the majority of the symptoms are from the secondary spread of muscle spasm and thus is more amenable to manual hands-on relief techniques.
A list of commonly used disc related terminology: Most of which are used interchangeably by people to describe their back pain.

- slipped disc
- ruptured disc
- bulging disc
- herniated disc
- crumbling disc
- disc compression
- displaced disc
- twisted disc
- pinched disc
- lumbago
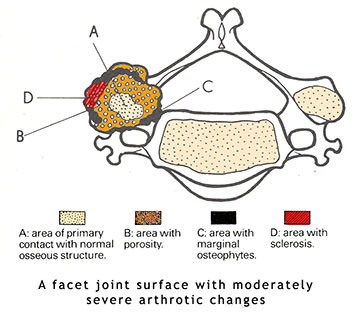
5. Joint related terminology
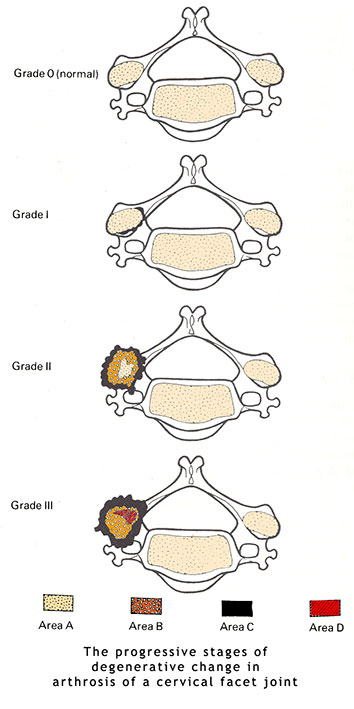
- Facet joint
The joints which act as guide rails and leverage points for movements of the spine. - Spondylosis
The long term result of compression and, or inflammation is the outgrowth of bone (spondylosis) around the perimeter of the facet joints. - Spondylitis
Inflammation of a facet joint normally from adjacent micro-trauma to the muscles and, or ligaments. - Spondylolisthesis
The forward slipping of a vertebra on anther. Usually due to a congenital defect known as a 'pars imperfecta'. The bridge of bone from the facet joint to the body of the vertebra (the pedicle) is born weak. The bridge remaining normally as tough fibrocartilage instead of becoming hard bone. - Arthrosis and Osteo-arthrosis
The long term degenerative changes which occur in chronically irritated and compressed facet joints - Osteo-arthritis of the spine
similar to spondylitis but chronic (long term) - Facet joint sprain and strain
A facet joint can be irritated by stretching it too far too suddenly. They can also be irritated by sudden compression and extreme rotation. - Facet joint displacement
When a joint has been injured, it will be held out of its natural position by the muscle spasm around it and by the adhesion which rapidly forms in the joints thus 'gluing' one or more facet joints together. this limits the range of motion and further, more widespread muscle tension develops in order to maintain some kind of balance of the spine. - Facet joint adhesion
The surfaces of the facet joints are lubricated by synovial fluid. This fluid is continuously secreted by the cartilage lining the joint. The fluid is maintained within a certain pressure range and can change density. When inflammation or repair is in progress the fluid becomes extra-sticky and can 'stick' the joint surfaces to each other. - Pinched facet joint
When a facet joint is placed into hyperextension i.e. bent back a facet joint can 'pinch' the capsular ligaments which surround the joint. This commonly produces nerve pain, pins and needles and numbness down the arm or leg. - Out of place joint
See facet joint adhesion above. - Subluxation
See facet joint adhesion above. Also a term used mainly by Chiropractors and Osteopaths to describe the character of partial dislocation which occurs due to injury and, or postural distortion of the spine. - Dislocation
Except in very extreme trauma this does not happen
6. Muscle related terminology
-
Muscle spasm
- If a postural muscle is irritated it will generally tighten in response. Sometimes the contraction response is so strong and goes on for so long that the muscle goes into a cramp. This is due to the muscle having run out of oxygen due to the contraction limiting the blood supply to it.
- Torn muscle
- A muscle can suffer complete rupture, but this is very rare. Usually a small percentage of the fibres which make up the muscle will 'come apart'. After some rest and appropriate treatment the fibres can heal like new.
- Sprained muscle
- A muscle sprain is a lesser form of tear. It can occur because of sudden stretching whilst over-contracting the muscle or from lifting too heavy a weight, too suddenly.
- Hypertonic muscle
- A muscle in a hyper-tense state. The muscle(s) have been either habitually worked too hard, kept in a tense, stabilising function, or chronically irritated by an underlying joint condition
- Tense muscle
- See hypertonic muscle
- Flaccid muscle
- A floppy, weak muscle, usually one of the skeletal muscles. These muscles weaken and lose reflex tone rapidly in response to irritation. Sometimes a flaccid muscle is produced by paralysis.
- Weak muscle
- Muscle which through under-use has become too weak for proper functionality.
-
 Musclebound
Musclebound
- See hypertonic muscle
- Inflammed muscle
- Muscle which has sustained enough damage to have become inflamed (repairing). The muscle can swell, become hot and too painful to operate. Best to rest and cool it with a cold, wet towel.
- Myositis
- See inflamed muscle
- Fibromyalgia
- Means fibrous/muscle/pain. This is a loose term and implies hardness, leatheriness accompanied by aching and pain
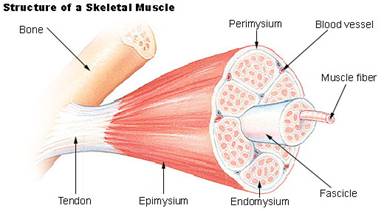
- Muscle pain
- Muscles register pain from various sources associated with the muscle. It can come from the chemical pain receptors which pick up signals from cramp and hypertonic states. There are other signals which emanate from the membrane which surrounds all muscles, the perimysium, when the muscle enlarges through exercise. The stretch on this tough membrane feels like stiffness. Muscle pain can come from damage and the stimulation of the repair process using both chemical and nerve pathways.
- Muscle ache
- See muscle pain
- Muscle stiffness
- See muscle pain
7. Tendon related terminology
- Tendonitis and
tendinitis
- An inflamed
tendon, usually due to repetitive over-use
or due to trauma such as a direct blow or
having suddenly overstretched (pulled)the
tendon. The inflammation rapidly spreads
along the tendon and its muscle and then
onto the joints which lay beneath it. Occasionally
the tendon can form a fibrous lump of scar
tissue at some point along its length. These
occur in specific areas of the body, such
as the palm and calf tendon. This can develop
into a trigger finger'.
Prolonged irritation and contracture of the tendon can lead to a condition known as Volkmanns' ischemic contracture and Duy-Putrens' contracture, although the latter condition is usually congenital in origin.
- An inflamed
tendon, usually due to repetitive over-use
or due to trauma such as a direct blow or
having suddenly overstretched (pulled)the
tendon. The inflammation rapidly spreads
along the tendon and its muscle and then
onto the joints which lay beneath it. Occasionally
the tendon can form a fibrous lump of scar
tissue at some point along its length. These
occur in specific areas of the body, such
as the palm and calf tendon. This can develop
into a trigger finger'.
- Inflamed tendon
- See tendonitis
- Pulled tendon
- See tendonitis
- Strained tendon
- See tendonitis
- Torn tendon
- Sometimes a tendon can be torn. As in the case of torn muscles, there are degrees of tear that occur in a tendon, from the micro-tear to the complete 'snap'. A torn tendon, given the right care can heal very rapidly. Special attention must be made to keep the circulation stimulated with light massage.
- Atrophied tendon
- The tendon and its associated muscle are short, taut and virtually non-contractable. Normally due to extreme under-use of a muscle. In some genetic disorders and central nervous system disorders atrophy will occur despite attempts at normal usage. This state is rare.
- Tendon contracture
- See tendonitis
- Tendon ischemia
- Occurs when the demands on blood supply exceed the available blood supply. Results in aching pain and cramp in the associated muscle and joints beneath.
- Trigger finger
- See tendonitis
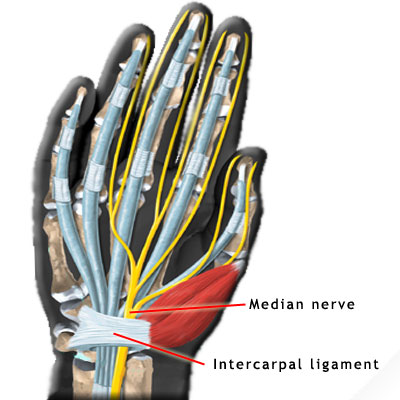
- Carpal tunnel syndrome
- Most often mistaken for a disc problem in the neck and vice-versa. The 'tunnel' passes beneath the intercarpal ligament of the palm of the hand. This ligament blends with the thenar muscles of the thumb and so are influenced greatly by the amount of tension resident in the thumb muscles. Pressure from displaced carpal bones, direct trauma to the palm and excessive tension in the long flexor muscles and their tendons as they pass beneath their bindings in the palm can all give rise to this condition. The result is usually pins and needles and, or numbness in the thumb, index, middle and half of the ring finger. Sometimes the thenar muscles become so congested that a throbbing pain can occur due to the blood supply away from the palm being impeded by the tension and swelling in and around the carpal tunnel.
8. Nerve related terminology
- Neuralgia
- Pain emanating from a nerve due to direct irritation of that nerve.
- Neuritis
- Inflammation of a nerve. For example optic neuritis and shingles.
- Neuropathy
- A group of nervous system disorders ranging from tertiary syphilis to diabetic neuropathy and lead poisoning.
- Pinched
nerve
- A nerve can be 'pinched' at various points along its route, each nerve having its own characteristic 'weak points'. The most common areas of pinching is at the exit of the nerves from the spine ( the foramina). They are pinched, compressed and pulled at these points.
- Compressed
nerve root
- See pinched nerve.
- Paralysed
nerve
- A nerve can be traumatised to the degree that it can no longer send signals to the muscles that it controls. This can be transient, as in 'dead leg' or permanent in severe trauma to the nerve. Poisons can also cause paralysis as well as central nervous system disorders. In the latter case the nerve signals cause contracture of the muscles.
- Pins and
needles
- The sensation of little needles pricking the skin and numbness occur principally due to often slight amounts of pressure on the nerve roots in the spine, or a greater amount of pressure somewhere along the route of the nerve. Such aberrant sensations are grouped under the descriptor 'parasthesiae'. The timing, intensity, permanence and variance from pins and needles to numbness and back again, all serve well to judge the severity of the case.
- Numbness
- See pins and needles
- Inflamed
nerve
- See neuritis
- Pulled nerve
- This is rare but can happen if a limb is stretched passively for example hanging by the arms form a tree branch can bring on parasthesia and even temporary paralysis.
- Crushed
nerve
- Can also result from a direct blow or intense squeezing as in industrial accidents, this condition is rare. If caught in the beginning there is hope of help. Nerves grow back and remake their connections but it can take many months, sometimes years to finally right itself. In cases of back pain, severe nerve pains from a gradually increasing 'squeezing of the nerve roots or at certain prone points along the route of the nerve e.g. sciatica, femoral neuralgia and radial neuralgia are most common.
I hope that you have found this glossary of back pain and commonly used terminology useful.
07925 616 753
Location: 8-10 Boston Place, Marylebone, London NW1 6QH
Next to Marylebone Station, Main line trains and Bakerloo line